Solid Tumors
CAF-tumors are sitting targets for NOX inhibition
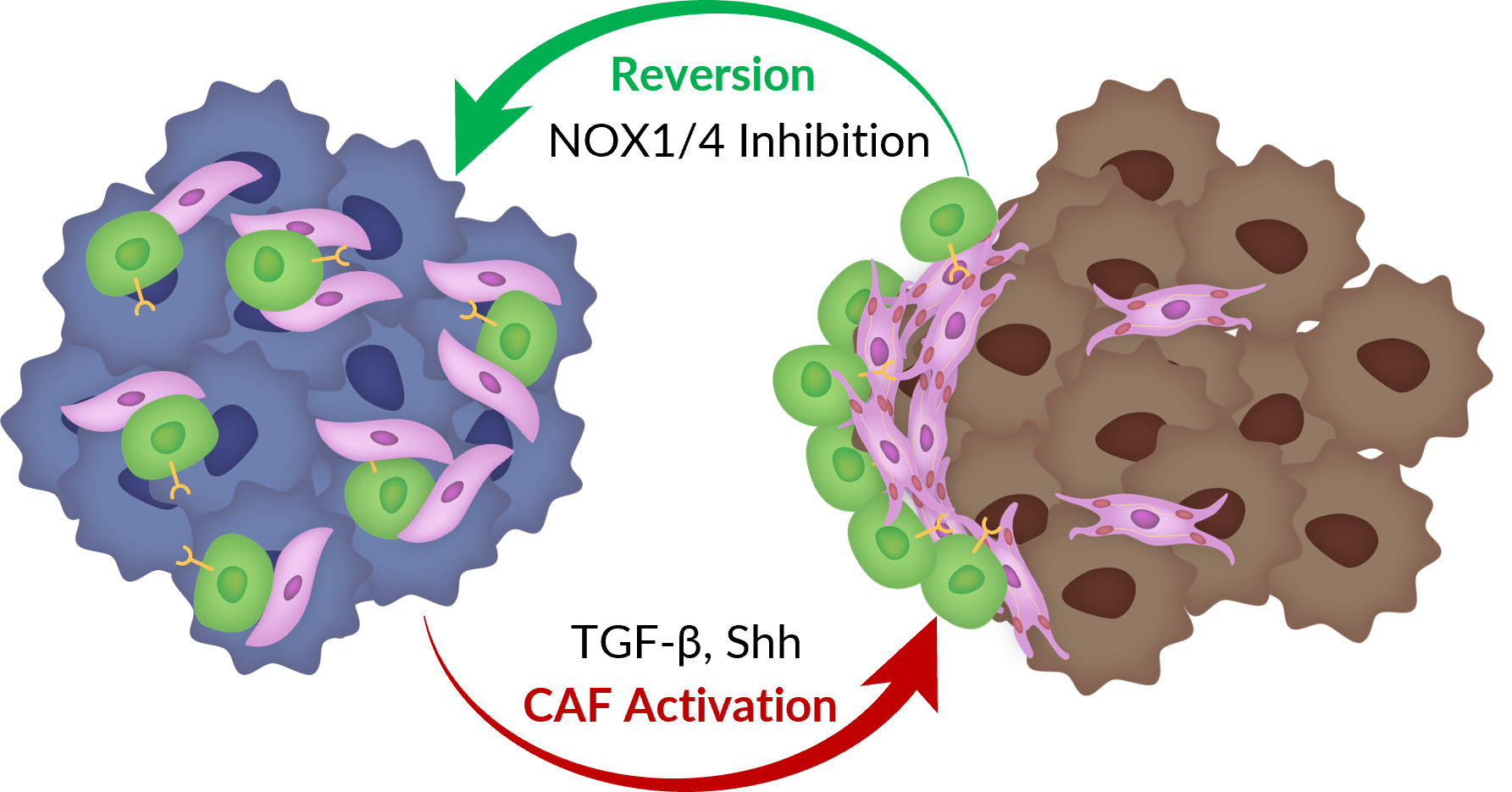
Cancer-associated fibroblasts are found in almost all solid tumors, however, their abundance varies across tumor types. Breast, prostate, and pancreatic tumors are CAF-rich, whereas brain, renal, and ovarian tumors exhibit fewer CAFs. CAFs can compose up to 80% of tumor mass in breast and pancreatic carcinomas. Solid tumors rich in CAFs are more resistant to immunotherapies and have low response rates on current standard of care. NOX1 and NOX4 expressed by CAFs are thought to trigger the reversion of CAFs (myofibroblasts) back to a dormant state.
This means NOX1/4 inhibition with setanaxib could re-sensitize the tumor microenvironment by improving the penetration of immune cells and ultimately boost efficacy of immunotherapies. A CAF-rich tumor microenvironment with high NOX4 expression is correlated to poor survival. Ph2 data in Head & Neck (SCCHN), but a preclinical data package is available in a breast tumor model with a follow-on compound. Calliditas believes there is significant partnering potential.
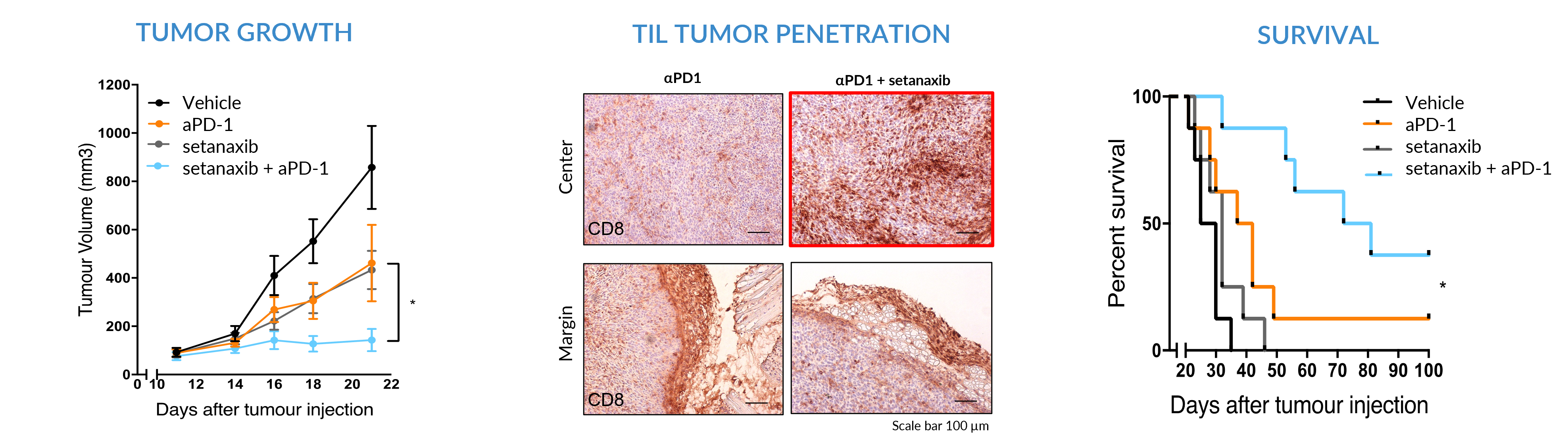
Preclinical Efficacy of Setanaxib + Anti-PD1 in CAF-Rich Solid Tumors
Legacy preclinical data in murine CAF-rich solid tumor models treated with setanaxib + anti-PD1 combination resulted in in statistically significant reduction in tumor volume, improvement in survival and immune cell penetration (TILs) to the tumor center.
These data drove the rationale to develop this combination in the Ph2 proof-of-concept study.
Phase 2 RCT in Head & Neck Cancer (SCCHN)
In May 2022, Calliditas announced that the first patient had been randomized in the company’s proof-of-concept Phase 2 study in patients with squamous cell carcinoma of the head and neck (SCCHN) with the NOX 1 and 4 inhibitor, setanaxib.
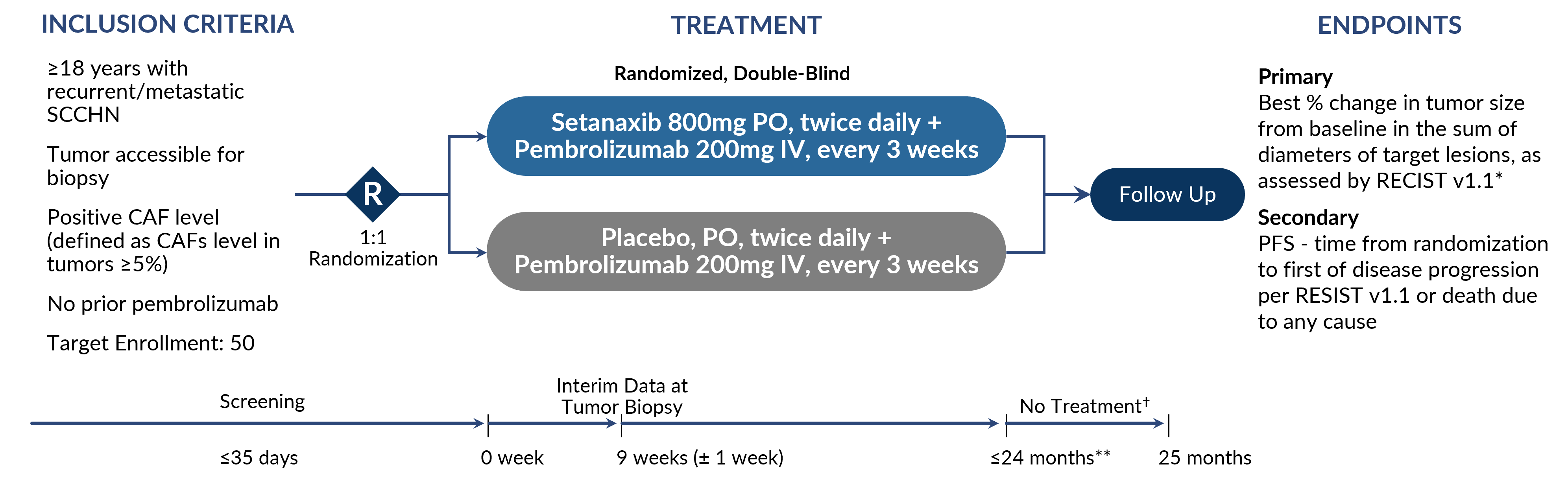
A full data readout is expected in 1H 2024.
Ph2 Positive Interim Data at 9 Weeks in Head & Neck Cancer (SCCHN)
July 2023 readout from 16 evaluable patients after 9 weeks of treatment. PFS: 7 of the 16 patients were progression-free with either stable disease or partial response (6 setanaxib arm: 1 placebo arm).
Biomarker Analysis: In a subset of 12 evaluable patients (tumor biopsies pre and post treatment) the transcriptomic analysis showed that the 2 top pathways impacted by the treatment were fibrosis‑related signaling pathways (the IPF signaling pathway and hepatic fibrosis/stellate cell activation pathway), supporting setanaxib’s modulatory effect on activated myofibroblasts.
Pathology Analysis: Increased immunological activity within tumors of patients treated with setanaxib, with favorable changes in specific pathology markers Foxp3 and PDL-1 CPS.
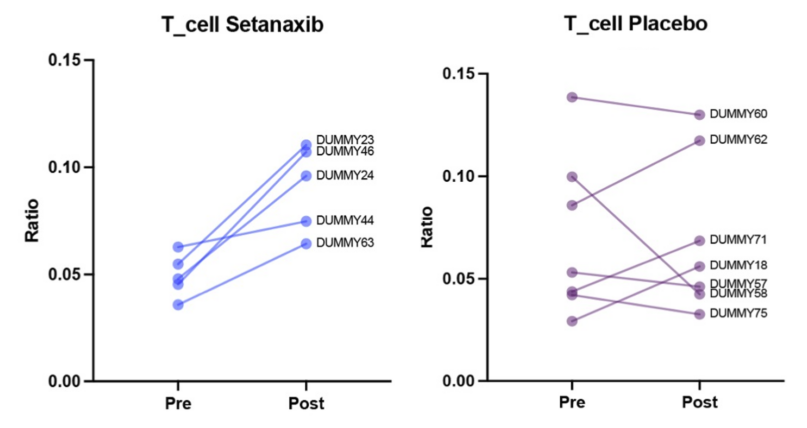
Increased Number of T-Cells Penetrating Tumor Patients on Setanaxib Treatment